How did more than 460K children in Florida lose their Medicaid health benefits?
TAMPA, Fla. - In Florida, more than 460,000 children lost their Medicaid health benefits after the COVID-19 pandemic.
Some lost coverage by mistake. Others were supposed to get a low-cost replacement that never arrived like Aurora and Luna Day.
Both sisters have serious medical conditions, and the legislature created a program to move them from state-run Medicaid (which covers children in lower income households) to an affordable alternative.
However, when state government cut off their Medicaid benefits, they discovered the affordable alternative did not kick in as lawmakers planned.
That's how their father, Donald, maxed out his credit cards, and why Donald, Aurora, and Luna had to move out of their home.

"It’s going to be very hard for me because I love this house so much," Aurora said.
Donald's a single father of two girls with Cystic Fibrosis—a digestive and lung disorder that requires a lot of attention.
"The treatments take 45 minutes for lung therapy. That’s twice per day. Every time they eat, they have to take medicine for that," he said.
And when they get sick, they can wind up in the hospital for days, or for Luna, nearly two weeks.
"I was crying because I missed her so much because she has always been in my life," Aurora said.
READ: Students return to Anna Maria Elementary School after Hurricanes Helene, Milton
Aurora and Luna and more than 460,000 other Florida minors lost access to Medicaid because rules changed after the pandemic, and the state determined their families earned too much income to keep their coverage.
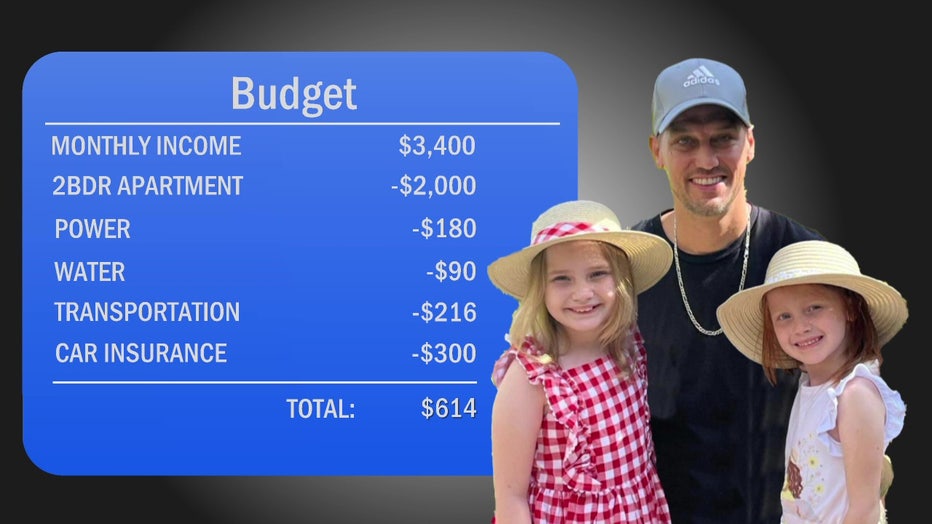
For context, Donald is bringing home around $3,400 a month. Zillow shows the median rent in the Tampa area is around $2,000 (close to what Donald was paying) plus power service.
"For electric, ballpark would be $180 on average. Then water was always like 90," he said.
Adding $50 a month for gasoline, and $300 a month in car insurance (which tends to cost more when you're in debt) leaves around $614 a month for food and everything else for Donald, Aurora, and Luna—or less than $7 a day for each of them before the girls lost Medicaid.
The legislature knew the Medicaid cuts were coming and passed a bill in 2023 to expand the state-subsidized KidCare insurance also known as Healthy Kids starting January of 2024. Aurora, Luna, and others losing Medicaid were supposed to be able to switch over for premiums of $15-$20 a month.
"Instead of moving forward we just go back, back, back," said Donald. "I was glad to see they were going to do something to help."
But then the state sent out letters that confused people.
For example, letters state that Medicaid is ending and the reason it's ending is just because it's ending, while also stating "you or a member of household remain eligible for Medicaid under a different Medicaid coverage group," while also noting "household income is too high to qualify for this program," and "you are receiving same type of assistance from another program."
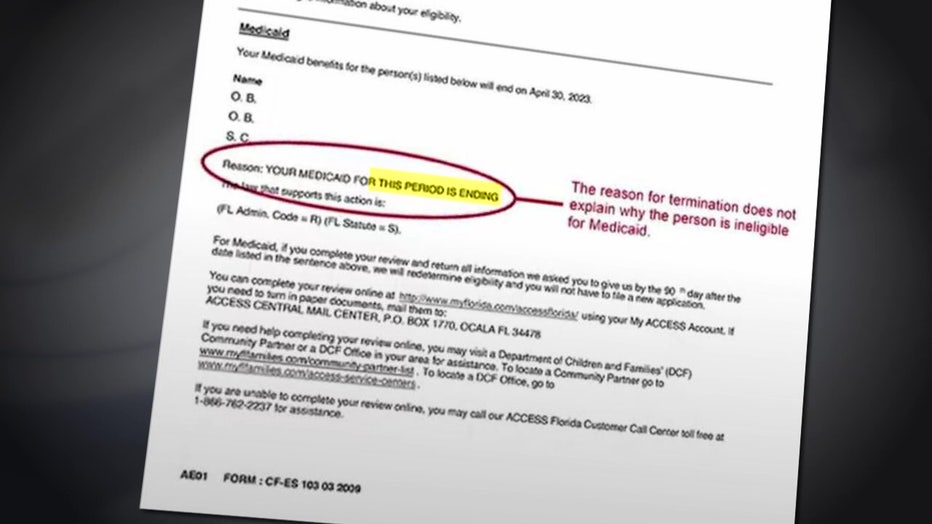
"Yeah, it’s just scattered. The words aren’t in the right place," Donald noted. "The way they word things is very weird."
That led some to take no action assuming they had some form of coverage when they didn't. It led others like Donald to apply for the KidCare expansion, which he discovered did not expand due to problems in the state's paperwork.
The federal government would pay 70% of the expansion after the state successfully submitted forms to the federal government.
However, Georgetown University Health Professor Joan Alker said Florida did not correctly submit the forms.
"States have to get what’s called a section 1115 waiver to expand Healthy Kids or their Chip program. It appears the state was not aware of that for quite some time. And when they finally did figure that out and got around to filing applications, they made a lot of mistakes," said Dr. Alker.
That delayed it for months. Then the state sued over federal rules requiring KidCare recipients to have at least 12 continuous months of coverage. That further stalled the implementation.
"This is a new protection Congress put in place, and it came into effect January 1st of 2024," Alker said. "Now Florida is the only state in the country that is challenging that new federal protection."
READ: Half of US teens spend over 4 hours daily on screens, CDC study finds
A federal judge in Tampa dismissed the state's lawsuit in May, but the state’s plan to appeal has kept the expansion on hold.
Given the need, Donald decided to get KidCare for both of his daughters 'without' the subsidies. Instead of paying $30-$40 per month as intended, he's paying $520 per month, plus co-pays for doctor visits, prescriptions, and more.
"Each kid takes a range of 8-10 different medicines. So it's just compiling, so it’s only $5, but when there’s 20-30 all of those $5-dollar payments, it adds up," said Donald. "It got to the point okay what are we eating right now? Can I borrow money for food."
That adds another $600-$700 to their monthly expenses and remember they only had around $614 a month for food and everything else.
The girls did get approved for social security payments, which helped a little at first, but social security told him the administration approved those payments by mistake. Now it is demanding more than $8,000 in repayments.
"At a time when our family needed help, I thought I was getting help, just to find out that they want to take the help back," Donald said.
That’s why they moved out of their home to live with Aurora and Luna's grandmother.
"There are a lot of days when I’m ready to give up... a lot of days like that. But I can't not with my kids. There's no giving up," Donald added.
In Florida, children only qualify for Medicaid if their family is within 133% of the federal poverty line. Those who come within 200% can get low-cost KidCare insurance. The expansion plan would expand to 300% of the federal poverty line.
STAY CONNECTED WITH FOX 13 TAMPA:
- Download the FOX Local app for your smart TV
- Download the FOX 13 News app for breaking news alerts, latest headlines
- Download the SkyTower Radar app
- Sign up for FOX 13’s daily newsletter

