Inside the COVID-19 ward at Tampa General Hospital: Precautions and progress
TAMPA, Fla. - Tampa General Hospital nurses Suzanne Dorner and Dylan McWherter weren't sure what to expect when their medical ICU unit transformed to the COVID-19 unit pretty much overnight.
"Most of July and August, every day I went in, I didn't sit down. I went in with these patients that were incredibly sick and incredibly unpredictable. These patients would come in breathing regular room air and then within 24 hours they need a breathing tube. So it was very unpredictable and you had to be flexible in every way," said McWherter.
"I read about the Spanish Flu of 1918 when I was a kid but I never could have pictured when I was going into nursing that that would actually happen," offered Dorner, the COVID ICU nurse manager.
There were a lot of unknowns.
"Were we going to get it? Were we going to pass it on to someone else? Was there someone who was going to get it outside of the hospital and bring it in?" listed McWherter.
Featured
Tampa General Hospital continues hydroxychloroquine study on healthcare workers
Since launching in the spring, a nationwide clinical trial hopes to answer whether hydroxychloroquine can prevent COVID-19 in healthcare workers treating coronavirus patients on the front lines.
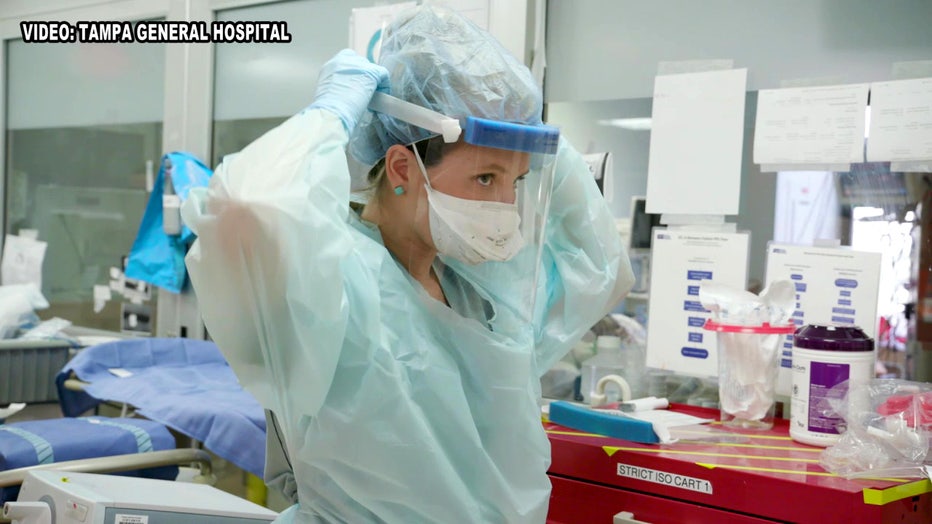
Tampa General Hospital – through their lens, for safety purposes – gave FOX 13 an exclusive view of the unit that only staff and patients see. The unit is set up specifically to treat patients of an unprecedented pandemic.
"Part of that response was making sure we had an adequate amount of ICU-capable rooms that were negative pressure, so basically kept the air inside the room and kept the clean air outside the room. It allowed our team to work more safely because of that negative-pressure environment," said John Couris, Tampa General's president and CEO.
"We've got isolation cabinets outside of each room, red magnets to signify that the patients are on strict isolation precautions. From a nursing perspective, we really had to change the way we practice nursing to limit the amount of time that nurses enter the room," Dorner continued.
Featured
Lab technician gives glimpse into COVID-19 test-kit processing lab
Next to the doctors and other healthcare workers saving lives daily are the BayCare medical technologists. BayCare labs are now processing all of their drive-through COVID-19 tests and they pulled back the curtain, giving FOX 13 a rare look inside their laboratories.
Dr. Jason Wilson, the associate medical director of Tampa General's emergency department, recalls when their now-empty disaster area was full.
"It was not uncommon that you would have all these folding chairs full of patients and then another area over here with folding chairs full of patients. I remember taking the elevators down, opening the door and there were just lines and lines of socially distanced chairs as far as you can see. That day a normal day in our emergency department, we might see 250 people in a day. We saw just down here 305 people plus the normal volume of patients," Dr. Wilson said.
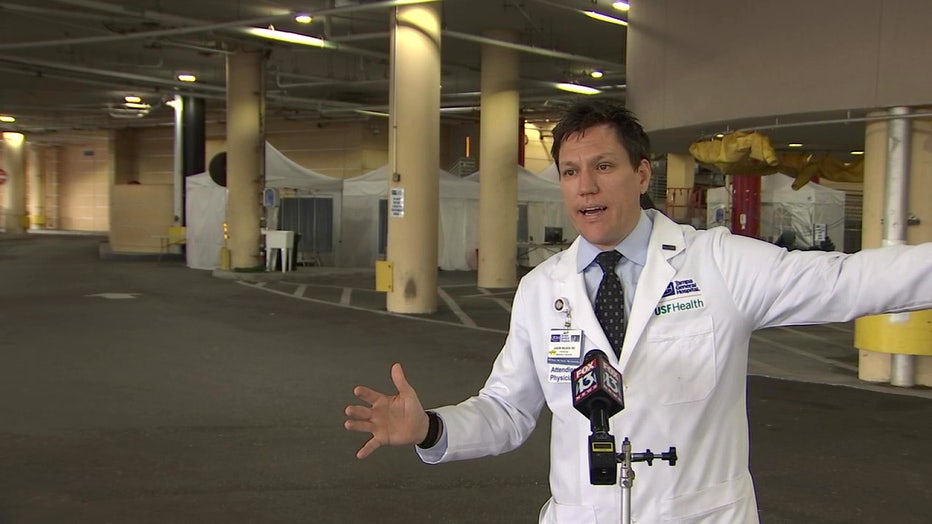
Dr. Jason Wilson explains the COVID-19 unit setup.
Over the past few months, it's been a learning curve.
"Some patients come in and they decline rapidly. Some in a matter of days or weeks and some just get better. I think it's just like any other patient with any other illness -- you're just trying to monitor them every hour to see which direction they are going," said McWherter.
Featured
Florida following country's upward COVID-19 case trend
COVID-19 cases in Florida rose sharply over the last few weeks and doctors are warning Floridians to avoid complacency in order to prevent another surge.
"What we did learn was less about the numbers and more about the unpredictable nature of the virus. So, for example, why does someone who comes into the hospital at 30 years old with no comorbidities, healthy, end up on a ventilator, and in some cases passing away? Like why does that happen versus somebody that comes in at 60 or 65 with two or three comorbidities and ends up leaving the hospital and is fine?" said Couris.
There's been some promising turns.
"Now we're educated on it. Our physicians are educated on it. Our staff is educated on it. We have an idea of what treatments we're doing," McWherter stated.
"At the height of COVID, probably had somewhere between 110 and 120 patients. Today we're sitting with 31 patients so it's a nice decline,” agreed Couris.
Featured
People fight 'pandemic fatigue' by going out, despite climbing cases
Positive COVID-19 cases are soaring across the nation, with 4,500 new cases reported Saturday in the state of Florida. But "you have to get out and live your life," some Bay Area residents say.
But there's also a message of caution.
"We're not out of the woods. We are holding our own. You take these masks off and we're going to be right back to where we started. Especially as we see the community start to go back out again,” Dr. Wilson warned.
"My sense is we're going to over time transition back to normal so people have to learn to co-exist with COVID-19,” Couris added. “There's no question about that.”





